In chapter 8. Hormones – Prof delves into Menopause Research and how it’s been sadly lacking for many years.
Chapter 8 – Hormones contd.
Menopause research…
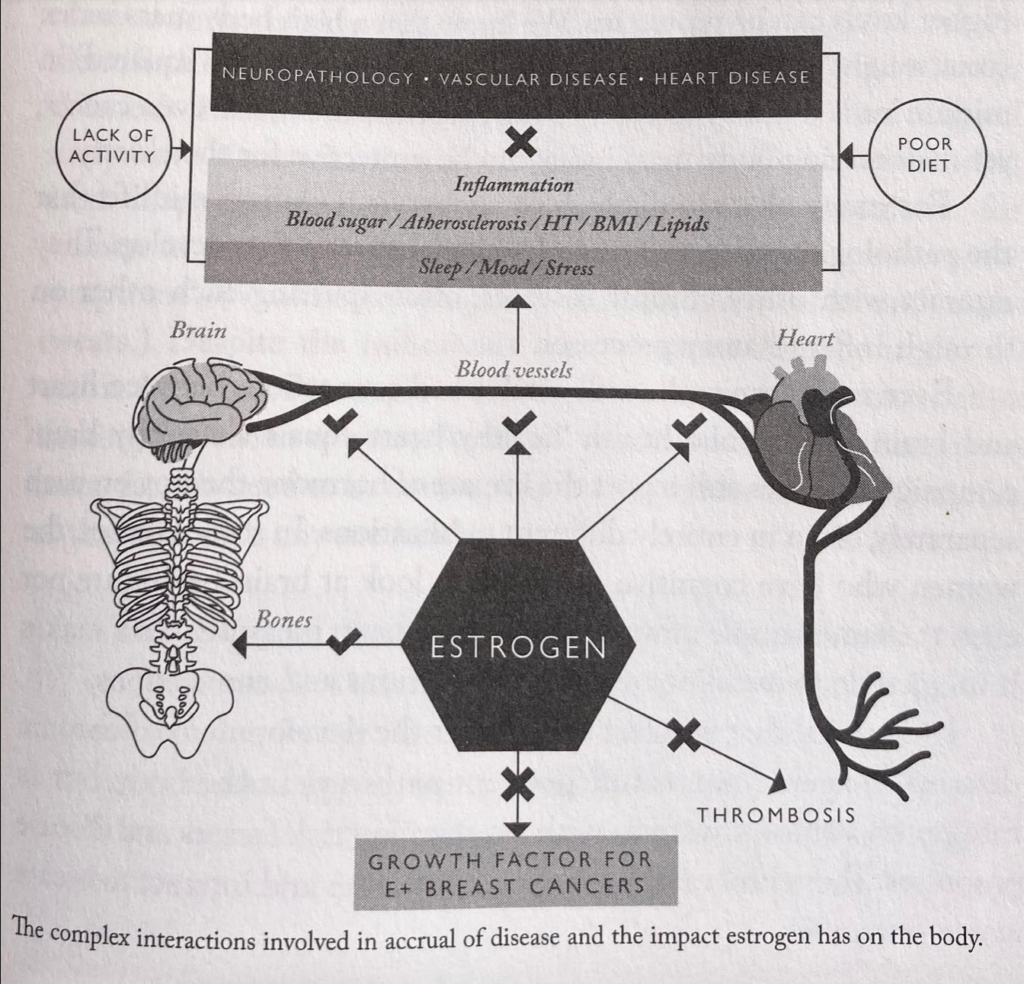
Endocrinologist Prof Henry Burger led much research in the field (study of female hormones) through the 1990s. His findings suggested that oestrogen might protect younger women from heart disease, stroke and peripheral vascular disease. This led to a view that hormone therapy might help counteract underlying diseases. Scientific papers showed beneficial effects of estrogens on cells (Bone, brain, vessels) and influence the “structure and function…and protect from oxidative stress, enhancing cell survival and plasticity (the ability to grow and adapt.”
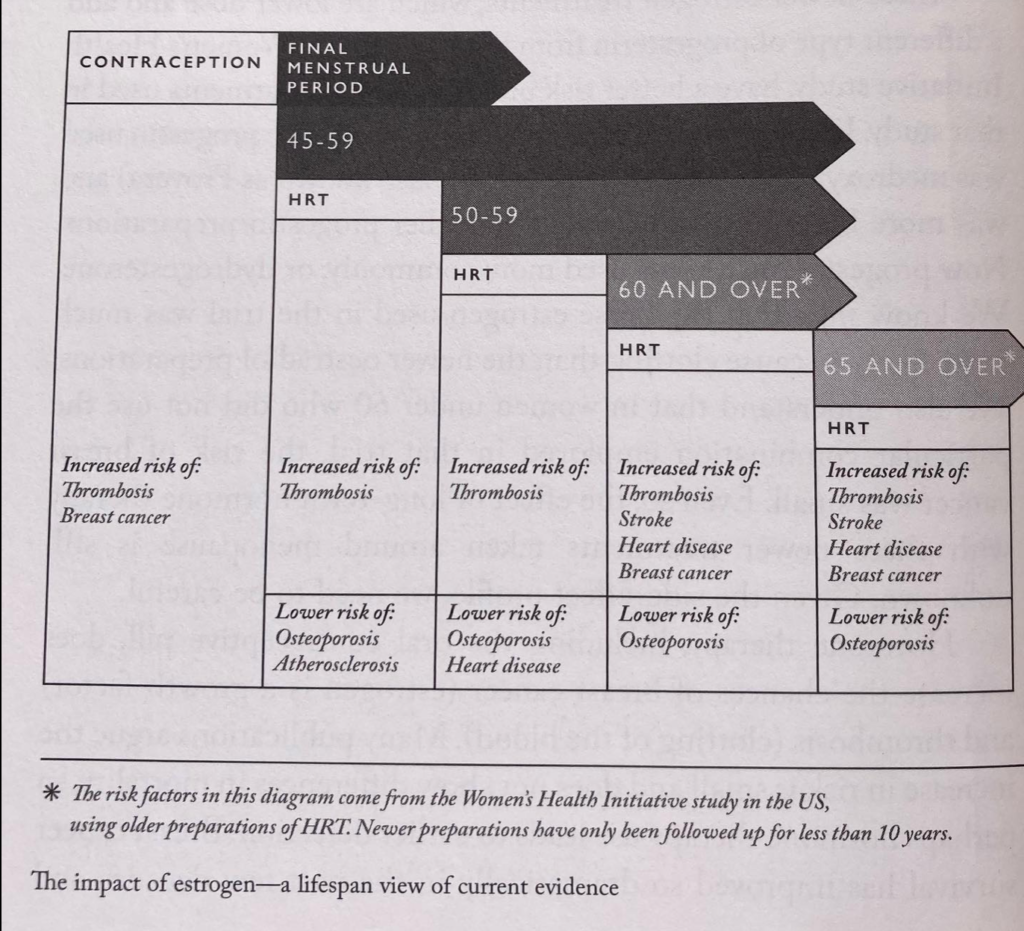
Low oestrogen has a causative link to osteoporosis – when combined with low calcium, being underweight and having low physical activity. Overall, prescribed hormone therapy has resulted in less heart disease, osteoporosis and dementia. And may help with depression, weight gain and even diabetes. However, studies show that late introduction of hormone therapy (after 60years and “far beyond menopause”) increased risks of blood clots and breast cancer. Plus, rather than improving outcomes for heart disease and dementia, it seemed to make it worse. The important thing to note here is early treatment is better than waiting until you’re post-menopausal.
Plus, newer oestrogen treatments that contain estradiol have a much better side-effect profile.
Ongoing studies are now looking at the benefit of HRT in younger cohorts and will examine long-term effects/ benefits in relation to diseases like dementia. 5-8 years of follow-ups from these studies show that “if you take the newer estrogen preparations with low-dose progesterone at the time of menopause, you have less atherosclerosis (clogging of the arteries) in your carotid vessels than if you did not take hormone therapy.
The 3-5 years funding cycles that are the norm in medical research limit the capacity to investigate long-term health outcomes. At last the “importance of determining changes of the course of life has been highlighted by the World Health Organisation’s department Gender, Health and Ageing section as crucial to women’s health.” It’s only since 2016 that studies have been required to have an equal number of male and female participants, so many of our current pharmaceutical treatments have been tested solely on men, or where women were involved, the results were not reported by sex.
The author notes that it is “crucial” to “consider the development of chronic diseases” not as independent pathways in the body, but as integrated, complex systems with overlapping risk factors and disease processes. These processes build on one another and interact to create worse outcomes.”
Early studies showing issues with HRT didn’t consider the age of the participants and therefore it was decades before the value was seen in the appropriate (menopausal) population, leaving many women understandably – but misguidedly – nervous of HRT even now.
I’ll delve deeper into types of HRT in the next post.