Everything you need to know about lymphedema.
Recently I wrote an article called ‘Health Benefits of Lymphatic Drainage), see 24th July 2016.
I briefly explained what ‘lymph’ is and how the lymphatic circulatory system works. In this article I touched on some causes of ‘lymphoedema’, i.e. congestion of lymph leading to fluid retention and swelling.
I’d like to explain a little more about why lymphoedema comes about and what we can do to relieve it and in particular focus on lymphoedema after breast surgery.
In a nutshell, Lymphoedema happens when lymph does not flow through the body in the way that it should.
When the lymph system is working properly, fluid, carrying proteins, fats and white blood cells away from the body’s tissues, is collected by lymphatic capillaries and is transported in one direction around our body. The right lymph duct collects lymph from the right arm and the right side of the head and chest and the left lymph duct collects lymph from both legs, the left arm, and the left side of the head and chest. It passes through lymph nodes where waste is filtered and eventually joins the subclavian veins where it mixes with our blood.
When the lymph system is damaged or blocked, fluid cannot drain from body tissues, allowing it to build up in the tissues and cause swelling, which in turn may cause other problems with the skin and soft tissues.
Lymphoedema is a progressive condition, which means it will get worse if it is not treated. Hence, it’s best to treat lymphoedema as early as possible to prevent it from worsening.
Lymphoedema can be either Primary or Secondary.
– Primary lymphoedema is a hereditary condition which happens as a result of an abnormal development of the lymphatic system, either at birth or later in life. It usually affects women more than men.
– Secondary lymphoedema is more common than primary lymphoedema and is caused by damage to the lymph system by infection, parasites, trauma, cancer, surgical removal of lymph nodes, radiation or scar tissue. It usually presents in the extremities, legs and feet, or in the case after breast surgery, in the arm and hand.
Stages of Lymphoedema
Stage 0: In this stage lymphatic drainage is reduced, but the remaining lymph vessels are working efficiently enough to compensate and the swelling will not be not obvious. This may occur post-operatively, but most people will only report mild discomfort or numbness, tingling or fullness in the affected limb. Compression garments and gentle lymphatic massage is used to successfully treat this stage of ‘latent’ lymphoedema.
Stage I: The lymph accumulates in the tissues, making the affected limb swell and feel heavy. Pressing on the swollen area leaves a slight indentation. Elevation and compression garments are used to manage this stage of lymphoedema to prevent progression to Stage II.
Stage II: The limb is swollen and feels heavy and the skin is ‘spongy’ to touch. Fibrosis (hardening of the connective tissue or fascia in the skin) might develop and skin will start to feel hard. Fat cells may swell, causing excessive fatty tissue to develop. Pressing on the swollen area won’t create an indentation as skin will bounce back. Complex (or Complete) decongestive therapy (CDT) is used to relieve the pressure on the skin.
Stage III: The limb will continue to swell until it is very large. The skin tissue may continue to harden and excessive fatty tissues are present. Lymphangitis (infection of the tissues) is now a possibility and untreated lymphoedema can lead to a further reduction in mobility or breakdown of the skin. Severe cases are known as Lymphostatic Elephantiasis. There is also a possibility of developing malignancy at this stage, known as lymphangiosarcoma. Patients can be treated with ongoing CDT or, in extreme cases, with surgery.
Diagnosing lymphoedema
A doctor or specialist will diagnose lymphoedema by taking a clinical history and a physical examination. They will usually take measurements and photographs of the affected limb and track these over time. They may also order an MRI scan (magnetic resonance imaging) to get a clearer picture. Other screening methods include water displacement, perometers (which measures the diameter of the limb), bioimpedance (or body composition) measures and special imaging called lymphoscintigraphy which observes the flow of lymph on x-ray by using a radioactive substance that is injected into the lymph.
In the Western world, lymphoedema most commonly occurs in women after breast cancer surgery.
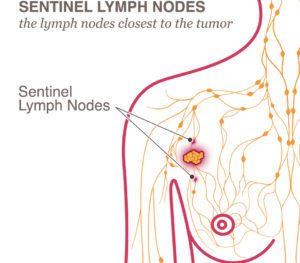 During breast cancer surgery (mastectomy or lumpectomy), some of the lymph nodes in the underarm (called axillary lymph nodes) may need to be removed. If the sentinel lymph node (the first lymph node that receives lymphatic drainage from a tumour) is the only one removed removed, there is less risk of lymphoedema occurring than if many lymph nodes are affected. These lymph nodes are then checked to see if cancer cells are present.
During breast cancer surgery (mastectomy or lumpectomy), some of the lymph nodes in the underarm (called axillary lymph nodes) may need to be removed. If the sentinel lymph node (the first lymph node that receives lymphatic drainage from a tumour) is the only one removed removed, there is less risk of lymphoedema occurring than if many lymph nodes are affected. These lymph nodes are then checked to see if cancer cells are present.
Surgical removal or treatment of these lymph nodes with radiation therapy may cause the lymphatic capillaries to become blocked, preventing lymph fluid from draining away. Lymphoedema post-mastectomy will usually develop within a few days to a few years of surgery.
Treating lymphoedema
There is no one ‘cure’ for lymphoedema unfortunately, but there are recommended treatments to help reduce the swelling and discomfort and return mobility to the affected limb.
Complex (or Complete) Decongestive Therapy (CDT). CDT is an intensive program that combines 4 different treatment approaches including; manual lymphatic drainage, compression, exercise and self-care. Initial “Active” care takes place daily, for an hour or two, over approximately 2 – 12 weeks. In the “Maintenance Phase” elastic compression garments are worn during the day and foam bandages are worn at night. Exercises are maintained and self-manual lymphatic drainage is done for 20 minutes per day.
Manual Lymphatic Drainage (MLD). A light skin-stretching massage technique that stimulates the lymphatic system
Compression. Layered foam bandaging or compression garments will help to control swelling.
Exercises. With compression, special exercises will help to pump lymph out of the swollen area. For example, exercises may include arm pumps, deep breathing and eventually lifting weights.
Skin Care. Clean and well-moisturised skin will help to prevent infections. Patients are advised to wear gloves whilst gardening, avoid having blood pressure and blood tests on that arm, avoid sunburn or any other trauma to the skin.
Endermologie treatment of lymphoedema
In a recent study, Doctors stated that “Endermologie therapy for a post-mastectomy upper limb lymphedema induced both objective improvement in the form of decrease upper limb swelling and subjective improvements in the form of decreased pain and improved the mobility of the affected limb. Upon the results of the current study Endermologie therapy can be recommended to patients with upper limb secondary lymphedema as a safe therapy without side effects.”
“The results of this study showed … the decrease of the arm circumference were significantly higher in the group (who) received the Endermologie treatment which may be due to facilitation of the lymphatic drainage from the affected limb by the use of the mechanized treatment head that allow continuous folding and unfolding of the skin under the continuous action of the rollers allowing for smooth and regulated deep tissue mobilisation.
As the viscosity of the subcutaneous fat layer decreases, blood flow and lymphatic drainage increase, facilitating the elimination of excess fluid and metabolites and improving overall cellular function … the Endermologie protocol induced additional subjective benefits reported by the patients in terms of an improvement in arm range of movement, decrease of accompanied pain and softening of fibrotic tissues of the swollen upper limb.”
A separate study compared Endermologie with manual massage and showed that: “Endermologie treatment has a 33% shorter treatment time than manual lymph drainage”.
What this means in lay-man’s terms: The gentle negative-pressure massage with Endermologie increases lymphatic drainage and mobilises fibrous skin tissue, reducing swelling and improving range of motion in the arm, decreasing pain and softening the skin. In fact, Endermologie was invented to create a more efficient and consistent massage technique for the treatment of scar tissue, so it is no surprise that clients report a faster outcome with Endermologie than with manual massage.
Note: It is important to see your health care provider if you have any symptoms of lymphoedema.